- I am autistic
- What is autism?
-
-
What is autism?
-
-
-
-
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
-
-
-
- Resources for you
-
-
Resources for you
A range of useful resources have been developed with autistic people. These can help with day to day activities and plans.
-
-
-
Autism: A guide for adults following diagnosis
This guide explains what autism is and how it can impact on an autistic person’s interaction with the world around them, providing practical hints and tips.
-
Advice sheets for autistic adults
On this page you will find downloadable links to a range of advice sheets on a variety of topics.
-
Autism Understanding & Accepting Scheme
If your organisation would like to register to become an ‘Autism Understanding & Accepting’ organisation and receive a personalised organisation / service certificate, please click here.
-
-
-
Adult Personal Profile
The profile can help people gain a better understanding of you and how they can help and support you more effectively.
-
Idioms Glossary
The glossary provides the meaning for various idioms.
-
Orange wallet
The orange wallet scheme aims to help neurodivergent people when travelling on public transport.
-
-
-
National Autism Team Resources Booklet
This resource booklet outlines the resources we have available on our website.
-
-
- Education
-
-
Education
A series of resources have been developed aimed at the key stages of education. These resources include information to increase understanding and awareness and to also help address many of the barriers that an autistic learner may face.
-
-
-
Further education
The resources are aimed at increasing understanding of autism for those working in FE and provides a practical handbook for autistic students.
-
Work based learning
The resources are aimed at increasing understanding of autism for those working in WBL and provides a practical handbook for autistic learners.
-
-
- Employment
-
-
Employment
A series of resources have been developed aimed at choosing the right career/job, securing and maintaining employment. These include practical tools for the autistic person and prospective/ current employers.
-
-
-
Master skills dictionary
Use the dictionary to search for terms that you wish to find the definitions of.
-
Personal skills builder
Create your personal skills list to assist you in your job search.
-
CV builder
Create your own CV here which you can save and download once complete.
-
-
-
Searching for work tool
To assist you in your job search, access our workbook here.
-
Resources for organisation helping you seek employment
This section includes resources that they may find useful when helping you seek employment.
-
Resources for employers
This section includes resources that your employer may find useful.
-
-
- Further resources/contacts
-
-
Further resources/contacts
This section includes resources and contacts that you may find useful.
-
-
-
My local contacts
Each Local Authority has a local Autism Lead that is the key contact for autism information, advice and guidance in that area.
-
Dewis Cymru
Dewis Cymru is the site to go to if you want information or advice about services within your area, as well as information on your well-being.
-
Integrated Autism Service
There are 7 Integrated Autism Services across Wales. They are a partnership between health and social care. Their primary focus is autistic adults who do not access statutory services or those adults seeking a diagnostic assessment.
-
-
-
Useful Links
Within this area of the website is a selection of other web resources that autistic people and those that care for them may find helpful.
-
-
- What is autism?
- I am a parent / carer
- What is autism?
-
-
What is autism?
-
-
-
-
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
-
-
-
- Information for parents & carers
-
-
Information for parents & carers
The resources within this section were developed in partnership with neurodivergent people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, understanding of autism and practical tools for parents and carers of neurodivergent people.
-
-
-
Autism: A Guide for Parents & Carers Following Diagnosis
This guide is aimed at increasing the knowledge, skills, and understanding of autism for those who support autistic children.
-
Autism: A Guide for Those Who Support Adults Following a Diagnosis
This guide is aimed at increasing the knowledge, skills, and understanding of autism for those who support autistic adults.
-
Parents & Carers Virtual Advice Sessions
Online information sessions for parents and carers, providing information about a range of topics relating to neurodivergence.
-
-
-
Autism videos for parents & carers
These films offer an insight into autism and offers practical hints and tips for parents and carers.
-
ASDinfoWales TV – Film for Parents & Carers
This film explores autism through the voice of autistic people, parent carers and professionals.
-
Living with Autism Film
This film captures the day to day lives of a range of autistic people.
-
-
-
Autism Understanding & Accepting Scheme
If your organisation would like to register to become an ‘Autism Understanding & Accepting’ organisation and receive a personalised organisation / service certificate, please click here.
-
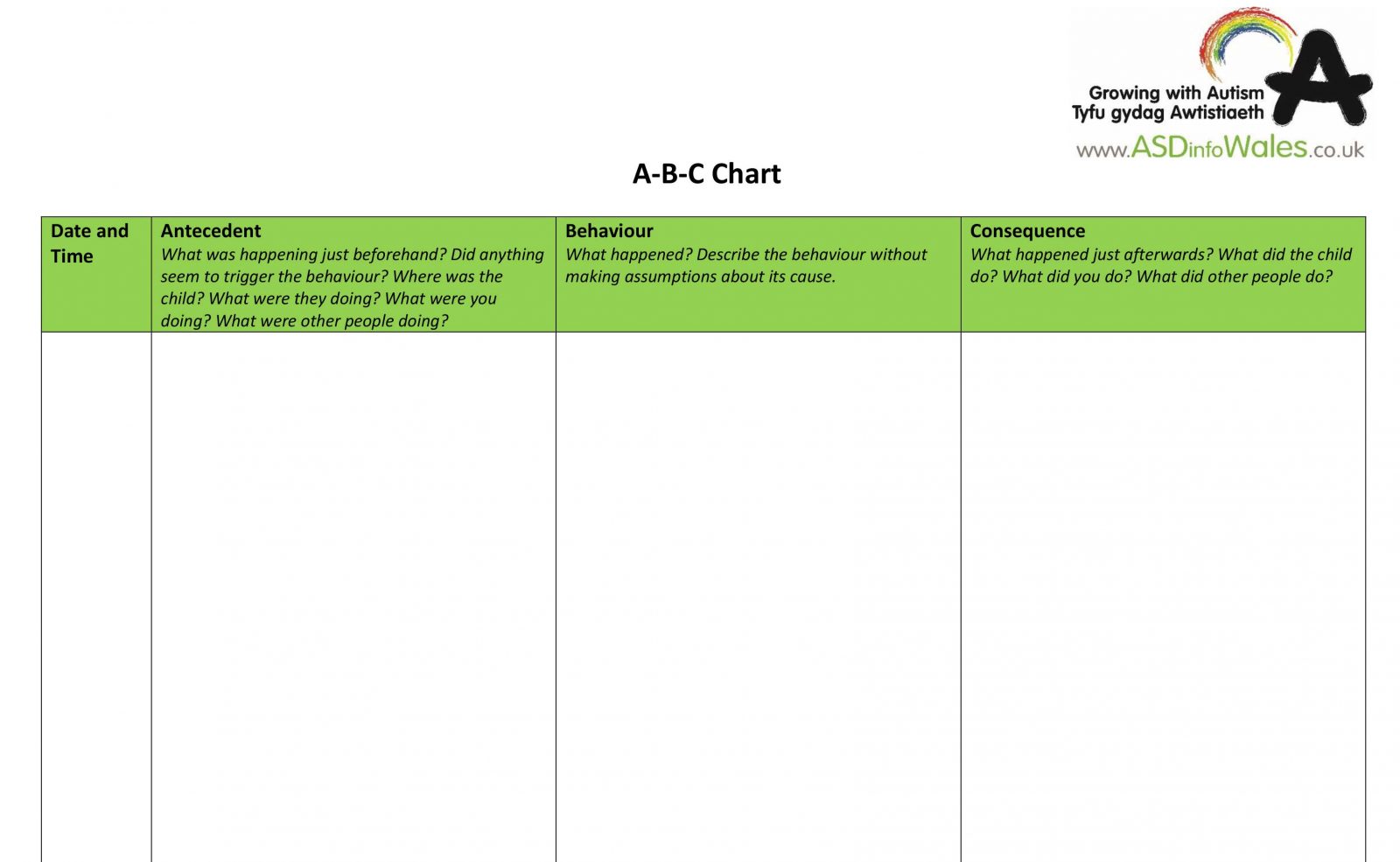
Child Advice Sheets
Here are practical advice sheets on a range of topics.
-
Child Personal Profile
The profile can help people gain a better understanding of your child and how they can help and support them more effectively.
-
-
-
Childrens Picture Cards
The picture cards can help create structure for your child’s day to day activities.
-
National Autism Team Resources Booklet
This resource booklet outlines the resources we have available on our website.
-
-
- Information for an autistic child
-
-
Information for an autistic child
This section contains information for autistic children.
-
-
-
Child Personal Profile
The profile can help people gain a better understanding of your child and how they can help and support them more effectively.
-
Childrens Picture Cards
The picture cards can help create structure for your child’s day to day activities.
-
Advice Sheets
Here are practical advice sheets on a range of topics.
-
-
- Information for young person / adult
-
-
Information for young person/adult
This section contains information for autistic young people and adults.
-
-
-
What is autism?
This section helps to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Education
The Learning about Autism programmes are aimed at raising awareness and understanding of autism across all educational settings.
-
Employment
A series of resources have been developed aimed at choosing the right career/job, securing and maintaining employment. These include practical tools for the autistic person and prospective/current employers.
-
-
-
Further resources/contacts
This section includes resources and contacts that you may find useful.
-
-
- Information for siblings
-
-
Information for siblings
This section contains information for the siblings of autistic children.
-
-
-
Teifi & Friends
These resources are aimed at pre-school children to help increase their awareness and understanding of autism.
-
Autism Superheroes
These resources are aimed at primary school children to help increase their awareness and understanding of autism.
-
Sgilti Lesson & Pupil Pledge
These resources are aimed at secondary school children to help increase their awareness and understanding of autism.
-
-
- Further resources/contacts
-
-
Further resources/contacts
This section includes resources and contacts that you may find useful.
-
-
-
My local contacts
Each Local Authority has a local Autism Lead that is the key contact for autism information, advice and guidance in that area.
-
Dewis Cymru
Dewis Cymru is the site to go to if you want information or advice about services within your area, as well as information on your well-being.
-
Integrated Autism Service
There are 7 Integrated Autism Services across Wales. They are a partnership between health and social care. Their primary focus is autistic adults who do not access statutory services or those adults seeking a diagnostic assessment.
-
-
-
Useful Links
Within this area of the website is a selection of other web resources that autistic people and those that care for them may find helpful.
-
-
- What is autism?
- Education
- What is autism?
-
-
What is autism?
-
-
-
-
This section helps to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
-
-
-
- I work in an early years setting
-
-
I work in an early years setting
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for those working in an early years setting.
-
-
-
Early Years Programme Overview
The Learning about Autism programmes are aimed at raising awareness of autism in all settings including non-maintained and maintained provision.
-
‘How to’ Early Years Video
Here is a video of the steps needed to undertake the Learning About Autism Early Years Scheme.
-
Self Evaluation Tools
There are two self-evaluation tools which help settings to identify current provision, practice, plan and monitor improvement.
-
-
-
Autism: A Guide for Early Years Settings
The Guide provides a framework to help early years settings become more autism aware and understanding and better meet the needs of autistic children in their care.
-
Early Years Setting staff scheme
The scheme is aimed at increasing the knowledge, skills, and understanding of autism of those working in an early years setting.
-
Autism Aware Certification
This scheme aims to provide an increased understanding of autism for all non-learning support staff.
-
-
-
Teifi & Friends
These resources are aimed at pre-school children to help the increase their awareness and understanding of autism.
-
Learning about Autism Early Years Setting Award
The Learning about Autism programme is a whole setting approach to improving awareness and understanding of the needs of autistic children.
-
Child profile
The profile can help people gain a better understanding of a child and how they can be helped and supported more effectively.
-
-
-
Childrens Picture Cards
The picture cards can help create structure for your child’s day to day activities.
-
Cue Cards
Cue cards can help autistic children to understand and follow instructions. Cue cards can be downloaded here.
-
Additional Resources
This section includes resources that you may find useful.
-
-
-
Early Years Case Study Videos
Here you can find case study videos that demonstrate how using the resources can improve practice in Early Years settings.
-
-
- I work in a primary school
-
-
I work in a primary school
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for those working in a primary school.
-
-
-
Introduction
The Learning about Autism programmes are aimed at raising awareness and understanding of autism across mainstream primary settings.
-
School Self-Evaluation Tool
The self-evaluation tool will help settings to identify current provision, practice, plan and monitor improvement.
-
Autism: A Guide Autism in Mainstream Primary Schools
The Guide provides a whole school framework to help schools become more autism aware and understanding and better meet the needs of autistic pupils.
-
-
-
Teaching Staff Training
The resources are aimed at increasing the knowledge, skills, and understanding of autism of teaching staff.
-
Learning Support Staff
The resources are aimed at increasing the knowledge, skills, and understanding of autism of learning support staff.
-
Autism Aware Certification
This scheme aims to provide an increased understanding of autism for all non-learning support staff.
-
-
-
Autism Superheroes
These resources are aimed at primary school children to help them increase their awareness and understanding of autism.
-
Learning about Autism Primary School Award
The Learning about Autism programme is a whole school approach to improving awareness and understanding of the needs of autistic pupils. A school can gain the award by completing the programme.
-
Child profile
The profile can help people gain a better understanding of a child and how they can be helped and supported more effectively.
-
-
-
Children Picture Cards
The picture cards can help create structure for your child’s day to day activities.
-
Cue cards
The picture cards can help create structure for your child’s day to day activities.
-
Additional Resources
This section includes resources that you may find useful.
-
-
- I work in a secondary school
-
-
I work in a secondary school
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for those working in a secondary school.
-
-
-
Introduction
The Learning about Autism programmes are aimed at raising awareness and understanding of autism across secondary school settings.
-
School Self-Evaluation Tool
The self-evaluation tools will help settings to identify current provision, practice, plan and monitor improvement.
-
Autism: A Guide Autism in Mainstream Secondary Schools
The Guide provides a whole school framework to help schools become more autism aware and understanding and better meet the needs of autistic pupils.
-
-
-
Secondary School teaching & learning support staff scheme
The resources are aimed at increasing the knowledge, skills, and understanding of autism of teaching and learning support staff.
-
Autism Aware Certification
This scheme aims to provide an increased understanding of autism for all non-learning support staff.
-
Sgilti Lesson & Pupil Pledge
These resources are aimed at secondary pupils to help increase their awareness and understanding of autism.
-
-
-
Learning about Autism Secondary School Award
The Learning about Autism programme is a whole school approach to improving awareness and understanding of the needs of autistic pupils.
-
Pupil Profile
The profile can help people gain a better understanding of a pupil and how they can be helped and supported more effectively.
-
Additional Resources
This section includes resources that you may find useful.
-
-
- I work in a further education institute
-
-
I work in a further education institute
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for those working in further education and to provide a practical handbook for autistic students.
-
-
-
Training film & resources for staff & students
These films and advice sheets provide information for tutors and teaching staff that support autistic students.
-
-
- I am a work based learning provider
-
-
I am a work based learning provider
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for those working in work based learning and to provide a practical handbook for autistic learners.
-
-
-
Training film & resources for staff & learners
These films and advice sheets provide information for tutors and teaching staff that support autistic learners.
-
-
- What is autism?
- Employment
- I am autistic
-
-
I am autistic
A series of resources have been developed aimed at choosing the right career/job, securing and maintaining employment. These include practical tools for the autistic person and prospective/current employers.
-
-
-
Master skills dictionary
Use the dictionary to search for terms that you wish to find the definitions of.
-
Personal skills builder
Create your personal skills list to assist you in your job search.
-
CV builder
Create your own CV here which you can save and download once complete.
-
-
-
Searching for work tool
To assist you in your job search, access our workbook here.
-
Exploring Employment Resource Booklet
This employment resource booklet for Autistic people provides practical information and signposts to useful employment resources. The booklet supplements the information provided at our Exploring Employment event.
-
Exploring Employment Event 2021
This section includes recordings of all workshops from our virtual employment event called ‘Exploring Employment: How to find and keep the job or career that’s right for you’. The event is for Autistic people of working age.
-
-
-
Employment Symposium Webinar 2020
This section includes recordings of workshops from our virtual employment symposium webinar. The symposium is aimed at employers, supported employment providers, and key employment staff.
-
Resources for organisation helping you seek employment
This section includes resources that they may find useful when helping you seek employment.
-
Resources for employers
This section includes resources that your employer may find useful.
-
-
- I am a parent / carer
-
-
I am a parent/carer
A series of resources have been developed aimed at helping autistic people in choosing the right career/job, securing and maintaining employment. These include practical tools for the autistic person and prospective/current employers.
-
-
-
Master skills dictionary
Use the dictionary to search for terms that you wish to find the definitions of.
-
Personal skills builder
Create your personal skills list to assist you in your job search.
-
CV builder
Create your own CV here which you can save and download once complete.
-
-
-
Searching for work tool
To assist you in your job search, access our workbook here.
-
Exploring Employment Resource Booklet
This employment resource booklet for Autistic people provides practical information and signposts to useful employment resources. The booklet supplements the information provided at our Exploring Employment event.
-
Exploring Employment Event 2021
This section includes recordings of all workshops from our virtual employment event called ‘Exploring Employment: How to find and keep the job or career that’s right for you’. The event is for Autistic people of working age.
-
-
-
Employment Symposium Webinar 2020
This section includes recordings of workshops from our virtual employment symposium webinar. The symposium is aimed at employers, supported employment providers, and key employment staff.
-
Resources for organisation helping you seek employment
This section includes resources that they may find useful when helping you seek employment.
-
Resources for employers
This section includes resources that your employer may find useful.
-
-
- I support autistic people seeking employment
-
-
I support autistic people seeking employment
A series of resources have been developed aimed at helping autistic people in choosing the right career/job, securing and maintaining employment. These include practical tools for the autistic person and prospective employers.
-
-
-
What is autism?
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Autism Understanding & Accepting Scheme
If your organisation would like to register to become an ‘Autism Understanding & Accepting’ organisation and receive a personalised organisation / service certificate, please click here.
-
Exploring Employment Resource Booklet
This employment resource booklet for Autistic people provides practical information and signposts to useful employment resources. The booklet supplements the information provided at our Exploring Employment event.
-
-
-
Exploring Employment Event 2021
This section includes recordings of all workshops from our virtual employment event called ‘Exploring Employment: How to find and keep the job or career that’s right for you’. The event is for Autistic people of working age.
-
Employment Symposium Webinar 2020
This section includes recordings of workshops from our virtual employment symposium webinar. The symposium is aimed at employers, supported employment providers, and key employment staff.
-
Autism: a guide for those who support adults following a diagnosis
This guide was developed in partnership with autistic people, parents and carers and professionals. It is aimed at increasing the knowledge, skills, and understanding of autism for those who support autistic adults.
-
-
-
Employment resources for individuals
A series of resources have been developed aimed at choosing the right career/job, securing and maintaining employment. These include practical tools for the autistic person.
-
Work based learning training provider resources
A series of resources have been developed aimed at WBL providers to gain greater skills, knowledge and understanding of autism and how to support autistic learners more effectively.
-
Further resources
This section includes resources and contacts that you may find useful.
-
-
- I am an employer
-
-
I am an employer
A series of resources have been developed aimed at employers to gain greater skills, knowledge and understanding of autism and how to support autistic employees more effectively.
-
-
-
What is autism?
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Employing an autistic person
These resources offer advice and guidance to employers on how best to support autistic employees in the workplace.
-
Autism Understanding & Accepting Scheme
If your organisation would like to register to become an ‘Autism Understanding & Accepting’ organisation and receive a personalised organisation / service certificate, please click here.
-
-
-
Living with autism film
This film captures the day to day lives of a range of autistic people.
-
Exploring Employment Resource Booklet
This employment resource booklet for Autistic people provides practical information and signposts to useful employment resources. The booklet supplements the information provided at our Exploring Employment event.
-
Exploring Employment Event 2021
This section includes recordings of all workshops from our virtual employment event called ‘Exploring Employment: How to find and keep the job or career that’s right for you’. The event is for Autistic people of working age.
-
-
-
Employment Symposium Webinar 2020
This section includes recordings of workshops from our virtual employment symposium webinar. The symposium is aimed at employers, supported employment providers, and key employment staff.
-
Autism: a guide for those who support adults following a diagnosis
This guide was developed in partnership with autistic people, parents and carers and professionals. It is aimed at increasing the knowledge, skills, and understanding of autism for those who support autistic adults.
-
Resources available for an autistic person
This section includes resources that your autistic employee may find useful.
-
-
-
Further resources / contacts
This section includes resources and contacts that you may find useful.
-
-
- I am autistic
- Community Services
- I work with children in health & social care
-
-
I work with children in health & social care
This section helps to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
-
-
What is autism?
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Community of Practice sessions
In this section, you will find recordings from our Community of Practice events, which focus on a range of different neurodivergent conditions, and issues that impact the neurodivergent community.
-
Autism Understanding & Accepting Scheme
If your organisation would like to register to become an ‘Autism Understanding & Accepting’ organisation and receive a personalised organisation / service certificate, please click here.
-
-
-
I work in Health care
This section helps to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
I work in Social Care
This section helps to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
The Birthday Party
This film highlights the way autism can present differently from person to person and outlines the signs of autism.
-
-
-
CAMHS Resource Toolkit & Quick Guide
This Resource Toolkit is for all professionals working in Specialist CAMHS but primarily for CAMHS clinicians working with neurodivergent children and young people, and their families to understand, explain and support wellbeing and practical outcomes.
-
-
- I work with young people / adults in health & social care
-
-
I work with young people/adults in health & social care
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for young people and adult health and social care professionals.
-
-
-
What is autism?
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Community of Practice sessions
In this section, you will find recordings from our Community of Practice events, which focus on a range of different neurodivergent conditions, and issues that impact the neurodivergent community.
-
Autism Understanding & Accepting Scheme
If your organisation would like to register to become an ‘Autism Understanding & Accepting’ organisation and receive a personalised organisation / service certificate, please click here.
-
-
-
I work in Health Care
This section helps to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
I work in Social Care
This section helps to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Living with Autism Film
This film captures the day to day lives of a range of autistic people.
-
-
- I work in housing
-
-
I work in housing
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for housing professionals.
-
-
-
What is autism?
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Housing Guide & certificated training scheme
This section is aimed at increasing the knowledge, skills and understanding of autism of housing services staff. And includes a comprehensive guide for housing staff based upon good practice and the Housing Act.
-
-
- I work in leisure & sport
-
-
I work in leisure & sport
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for those working in sport and leisure services.
-
-
-
What is autism?
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Autism Understanding & Accepting Scheme
If your organisation would like to register to become an ‘Autism Understanding & Accepting’ organisation and receive a personalised organisation / service certificate, please click here.
-
-
- I work in the emergency services
-
-
I work in the emergency services
The resources within this section were developed in partnership with autistic people, parents and carers and professionals. The resources are aimed at increasing the knowledge, skills, and understanding of autism for those working in the emergency services.
-
-
-
What is autism?
This page highlights key resources on our website which help to build a better understanding of autism. A range of resources have been developed in partnership with autistic people, parents and carers and professionals that clearly explain what autism is and how it affects autistic people’s interaction with the world around them.
-
Emergency Services Training Film
This section is aimed at increasing the knowledge, skills and understanding of autism for the emergencies services.
-
-
- I work with children in health & social care
- Integrated Autism Service